What Is Yersinia pestis and How Does It Spread?
Although the plague caused by Y. pestis may seem like a disease of the past, researchers continue to study its transmission and how to best treat it.
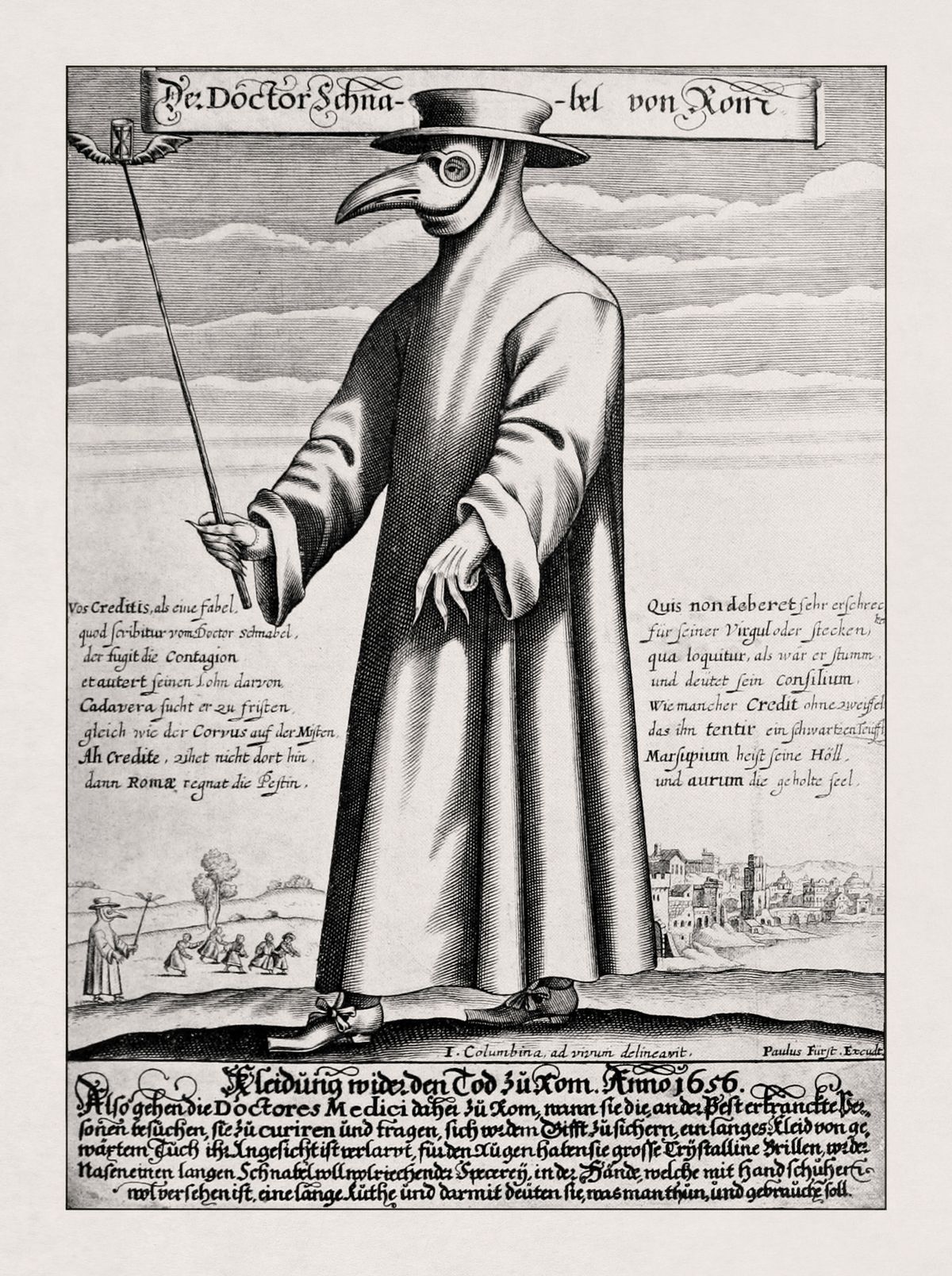
Yersinia pestis is a bacterium responsible for the plague, a serious infectious disease that has caused several deadly epidemics throughout human history.1-3 The most well-known epidemic, often referred to as “the Black Death,” arrived at a Sicilian port in 1346, likely through ships originating from Central Asia. Over the next five to seven years, the disease spread across Europe, Asia, and northern Africa, claiming the lives of 25 to 50 million people—about 30 percent of the world’s population. Notably, plague still occurs today, though humans no longer experience widespread outbreaks.
How Does Yersinia pestis Spread?
The most commonly studied and identified mode of Y. pestis transmission is through rat fleas, where the bacteria colonize the fleas' digestive tract.4 When a flea takes a blood meal from its host, often a rodent, it regurgitates the bacteria, transferring it to the unsuspecting animal. Humans can be infected with Y. pestis through bites from either fleas or an infected mammalian host. However, rodents and their fleas are not the only vectors of this disease. Although it has long been known that plague can be transmitted by handling tissue from infected humans, recent findings suggest that human ectoparasites, like lice, may also play a role in spreading the disease.5
The human ectoparasite hypothesis
Much of the historical support for the human ectoparasite hypothesis stems from observations during the Black Death.6 High mortality rates, particularly within single households, suggest a more direct human-to-human transmission pattern rather than one involving a rodent intermediary. Additionally, the climate in northern Europe likely did not support a large rat population, and there were no significant reports of widespread rat deaths, or rat falls, as seen in other plague epidemics.
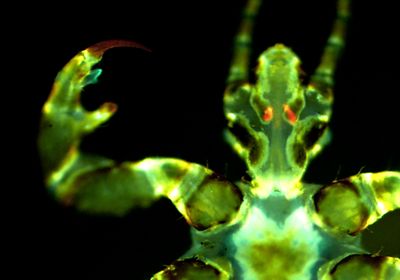
Recently, some scientists have put the human ectoparasite hypothesis to the test. Joe Hinnebusch is a recently retired NIH microbiologist who investigated plague transmission, infection, and immunity. In his lab, human lice and squirrel fleas fed on blood infected with Y. pestis.7,8 The researchers then provided these ectoparasites with sterile blood to feed on. They discovered that the previously sterile blood became contaminated with the bacteria, indicating that these colonized ectoparasites, particularly lice, could potentially infect their human hosts during feeding.
Human lice are known to transmit other diseases, like typhus, but they do so through their feces, not bites. “This infection via the louse bite was new, never been reported. So that was fairly significant,” Hinnebusch said. His lab also discovered that lice with Y. pestis-colonized Pawlowsky glands—a pair of salivary glands in the louse's head—transmit the bacteria more effectively than those with Y. pestis colonizing their digestive tract.
Although Hinnebusch emphasized that rodent fleas remain the primary vector for plague transmission, his research raises questions about the role of human lice in other plague outbreaks. These findings could also have public health implications, especially in regions where plague still occurs, such as East Africa, Central East Africa, and Madagascar. A deeper understanding of Y. pestis transmission routes could help reduce the spread of the disease.
Plague Symptoms
Although often thought of as one illness, there are actually three main types of plague: bubonic plague, septicemic plague, and pneumonic plague.1,3,9
A person with bubonic plague develops sudden fatigue, dizziness, high fever, limb pain, and headache three to seven days after exposure to Y. pestis. They will also experience significant lymph node inflammation. The nodes nearest the location of the bite will develop characteristic buboes—from which bubonic plague takes its name—marked by tense, painful, warm swelling that can grow up to 10 centimeters.3,9
The second form of Y. pestis infection is septicemic plague. In this manifestation, Y. pestis multiplies primarily in the blood rather than the lymph nodes. These patients can develop tissue necrosis and can rapidly deteriorate into shock.3,9
Lastly, pneumonic plague uniquely spreads through human-to-human contact via droplet particles. Patients with pneumonic plague will initially develop vague, flu-like symptoms before experiencing sudden high fever, breathing-associated chest pain, shortness of breath, and cough that brings up blood.3,9
Plague Treatment and Prevention
Antibiotics
The key to treating plague lies in prompt diagnosis and antibiotic administration. Commonly used medications are gentamicin and streptomycin, which are members of the aminoglycoside class of antibiotics.9 Aminoglycosides work by preventing bacteria from synthesizing proteins.11
While antibiotics eradicate Y. pestis in most cases, scientists have identified multi-drug resistant strains.12 Concerns over bioterrorism or the re-emergence of the plague globally have prompted scientists to look for alternative methods for prevention and treatment, particularly vaccines.
Vaccines
Experimentation with plague vaccines began in 1895 when Alexandre Yersin started immunizing test animals with heat-killed strains of Y. pestis.13,14 Shortly thereafter, scientists began experimenting with live-attenuated vaccines, which use a weakened form of Y. pestis that is not harmful but is still potent enough to trigger the body’s immune system. A live-attenuated vaccine using the EV76 strain of Y. pestis is still used in some countries today, but it is not favored in the US due to concerns that the bacteria could revert to a more infectious form. During the Vietnam War, US soldiers were given a plague vaccine containing Y. pestis that had been killed using formalin, a mixture of formaldehyde and methanol. While this vaccine appeared to successfully ward off bubonic plague, it did not provide protection against other forms of the disease and was also associated with adverse reactions. Currently, the preferred area of focus in Y. pestis vaccination is the development of a subunit vaccine, which uses specific components of the infectious agent, called antigens, to trigger the body’s immune system.15 The F1 protein, found on the capsule surrounding Y. pestis, and the low calcium response V (LcrV) protein, which assists Y. pestis in invading host cells, are frequently used as antigens in subunit vaccination experiments.
FAQs
What is Yersinia pestis?
- Yersinia pestis is a bacterium that causes the plague, a serious illness that can be deadly without prompt treatment.
What are the types of plague?
- There are three main types of plague: bubonic, septicemic, and pneumonic.
What are plague symptoms?
- All three types of plague cause flu-like symptoms and high fevers. Bubonic plague is associated with painful swelling of the lymph nodes. Septicemic plague causes tissue necrosis and shock. Pneumonic plague causes a lung infection associated with chest pain, shortness of breath, and bloody sputum.
How does the bubonic plague spread?
- Bubonic plague is spread by bites from infected fleas and their rodent hosts. However, recent research indicates that human lice and fleas can also contribute to the spread of disease.7,8
- Pneumonic plague is spread by contact with infected droplets.
Is there a bubonic plague treatment?
- Bubonic plague is treated with antibiotics like gentamicin and streptomycin. Research on plague vaccines remains an active field.
- Perry RD, Fetherston JD. Yersinia pestis--etiologic agent of plague. Clin Microbiol Rev. 1997;10(1):35-66.
- Barbieri R, et al. Yersinia pestis: The natural history of plague. Clin Microbiol Rev. 2020;34(1):e00044-19.
- Glatter KA, Finkelman P. History of the plague: An ancient pandemic for the age of COVID-19. Am J Med. 2021;134(2):176-181.
- Dewitte A, et al. A refined model of how Yersinia pestis produces a transmissible infection in its flea vector. PLoS Pathog. 2020;16(4):e1008440.
- Jullien S, et al. Plague transmission from corpses and carcasses. Emerg Infect Dis. 2021;27(8):2033-2041.
- Dean KR, et al. Human ectoparasites and the spread of plague in Europe during the Second Pandemic. PNAS. 2018;115(6):1304-1309.
- Bland DM, et al. Yersinia pestis can infect the Pawlowsky glands of human body lice and be transmitted by louse bite. PLoS Biol. 2024;22(5):e3002625.
- Bosio CF, et al. Comparison of the transmission efficiency and plague progression dynamics associated with two mechanisms by which fleas transmit Yersinia pestis. PLoS Pathog. 2020;16(12):e1009092.
- Prentice MB, Rahalison L. Plague. Lancet. 2007;369(9568):1196-1207.
- Mussap CJ. The plague doctor of Venice. Intern Med J. 2019;49(5):671-676.
- Krause KM, et al. Aminoglycosides: An overview. Cold Spring Harb Perspect Med. 2016;6(6):a027029.
- Lei C, Kumar S. Yersinia pestis antibiotic resistance: A systematic review. Osong Public Health Res Perspect. 2022;13(1):24-36.
- Sun W. Plague vaccines: status and future. Adv Exp Med Biol. 2016;918:313-360.
- Rosenzweig JA, et al. Plague vaccines: New developments in an ongoing search. Appl Microbiol Biotechnol. 2021;105(12):4931-4941.
- Aftalion M, et al. Rapid induction of protective immunity against pneumonic plague by Yersinia pestis polymeric F1 and LcrV antigens. Vaccines. 2023;11(3):581.